Heart health rarely announces itself with drama. For most people, problems build quietly—through habits that feel normal, symptoms that seem minor, and assumptions that delay action. To know heart health is not about memorizing medical terms or tracking every metric obsessively. It is about understanding which signals matter, which risks are avoidable, and which choices compound over time—especially in a world where sedentary work, processed diets, chronic stress, and rising metabolic disease have become the default.
This guide focuses on what deserves attention and what often gets dismissed too easily. It separates useful vigilance from unnecessary anxiety, and personal responsibility from medical guidance—so readers can make informed, proportionate decisions.
Why knowing heart health matters more now
Cardiovascular disease remains the leading cause of death globally, with onset occurring earlier than in previous generations. In India and many other regions, heart disease increasingly affects people in their 30s and 40s, driven by hypertension, type 2 diabetes, obesity, and tobacco exposure. Globally, similar trends are linked to ultra-processed foods, reduced physical activity, and persistent stress.
To know heart health today means recognizing that risk is no longer confined to old age or family history alone. It is shaped by daily patterns—sleep, diet, movement, and stress regulation—long before symptoms appear.
The foundations you should understand clearly
What “heart health” actually includes
Heart health is not a single number or test. It reflects how well the cardiovascular system delivers oxygen and nutrients, regulates pressure and rhythm, and adapts to physical and emotional demands. Core components include:
- Blood pressure (both systolic and diastolic)
- Cholesterol balance, including LDL cholesterol and HDL cholesterol
- Blood sugar control
- Heart rhythm and structural integrity
- Inflammatory status and vascular flexibility
Understanding these elements helps people interpret test results without panic or complacency.
What you should never ignore
Persistent or unusual chest discomfort
Chest pain does not always feel dramatic. It may present as pressure, tightness, heaviness, or burning—sometimes mistaken for acidity or muscle strain. Pain that:
- Occurs with exertion
- Radiates to the arm, jaw, neck, or back
- Improves with rest but returns with activity
should always be evaluated promptly.
Shortness of breath without clear cause
Breathlessness during routine activity or at rest can indicate reduced cardiac efficiency, fluid buildup, or rhythm issues. When it appears without infection or lung disease, it deserves attention.
Swelling in feet or ankles
Gradual swelling can signal fluid retention related to reduced heart pumping capacity, especially when combined with fatigue or weight gain.
Repeated dizziness or fainting
These episodes may point to rhythm disturbances or blood pressure regulation problems.
Family history combined with symptoms
Genetics alone does not guarantee disease—but family history plus symptoms significantly raises relevance.
What people often worry about unnecessarily
Occasional palpitations
Brief awareness of heartbeat after caffeine, stress, or poor sleep is common and often benign. Persistent, irregular, or symptomatic palpitations are different—and worth assessment.
Single abnormal reading
One high blood pressure or cholesterol result does not define disease. Trends over time matter more than isolated values.
Fitness tracker fluctuations
Wearables can be useful for awareness but are not diagnostic tools. Data should inform conversations with clinicians, not replace them.
The silent risks that deserve more respect
High blood pressure
Often symptom-free, hypertension quietly damages arteries, kidneys, eyes, and the heart itself. Many people discover it only after complications arise.
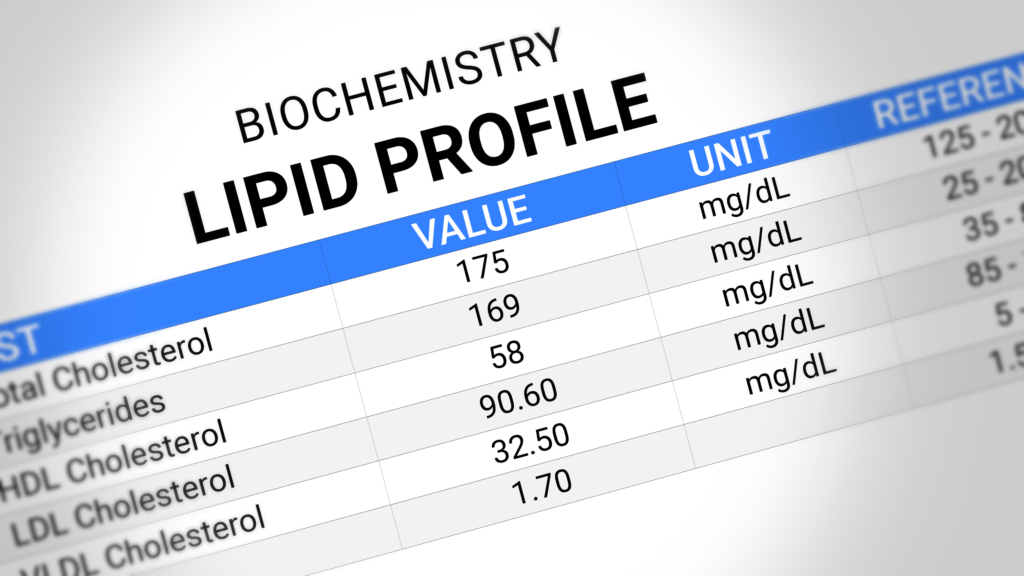
High cholesterol
Elevated LDL cholesterol contributes to plaque formation even in young adults. Normal weight does not guarantee healthy lipid levels.
Chronic stress
Sustained stress alters hormonal balance, raises blood pressure, disrupts sleep, and promotes inflammatory pathways that affect the heart.
Poor sleep
Consistently short or irregular sleep increases cardiovascular risk independent of diet or exercise.
Lifestyle factors that matter more than most realize
Diet: patterns over perfection
Heart-supportive eating emphasizes:
- Whole grains, fruits, vegetables, legumes
- Nuts, seeds, and healthy fats
- Limited ultra-processed foods and added sugars
It is consistency—not extremes—that influences outcomes.
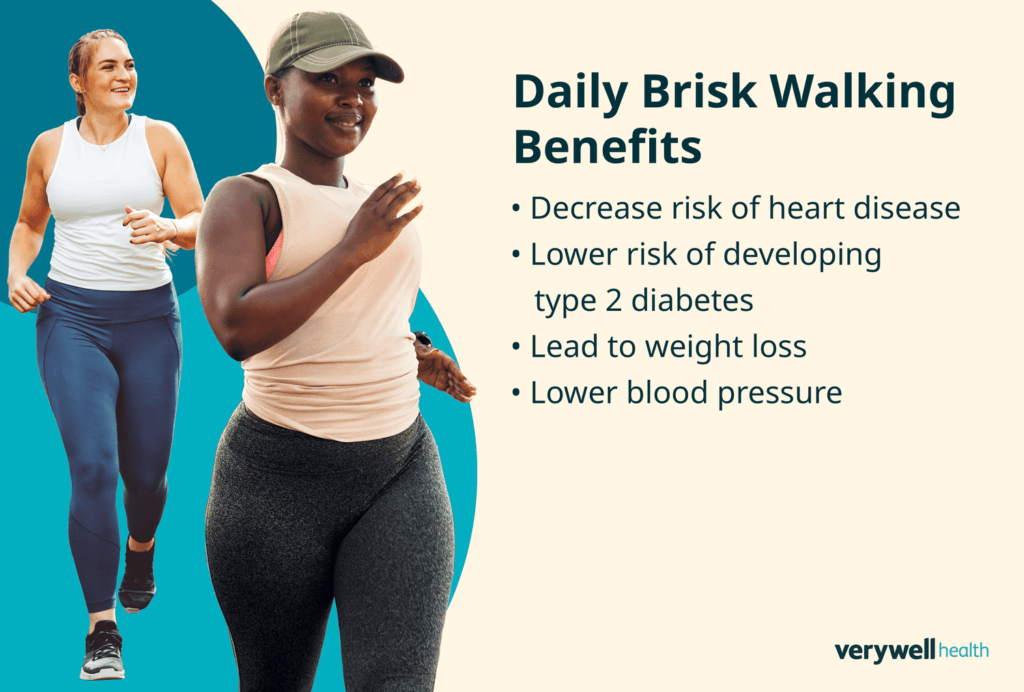
Physical activity: regularity beats intensity
Moderate activity most days improves vascular function, insulin sensitivity, and blood pressure regulation more reliably than sporadic intense workouts.
Tobacco and alcohol
Smoking remains one of the strongest modifiable risk factors. Alcohol’s “protective” reputation is increasingly questioned; moderation is essential.
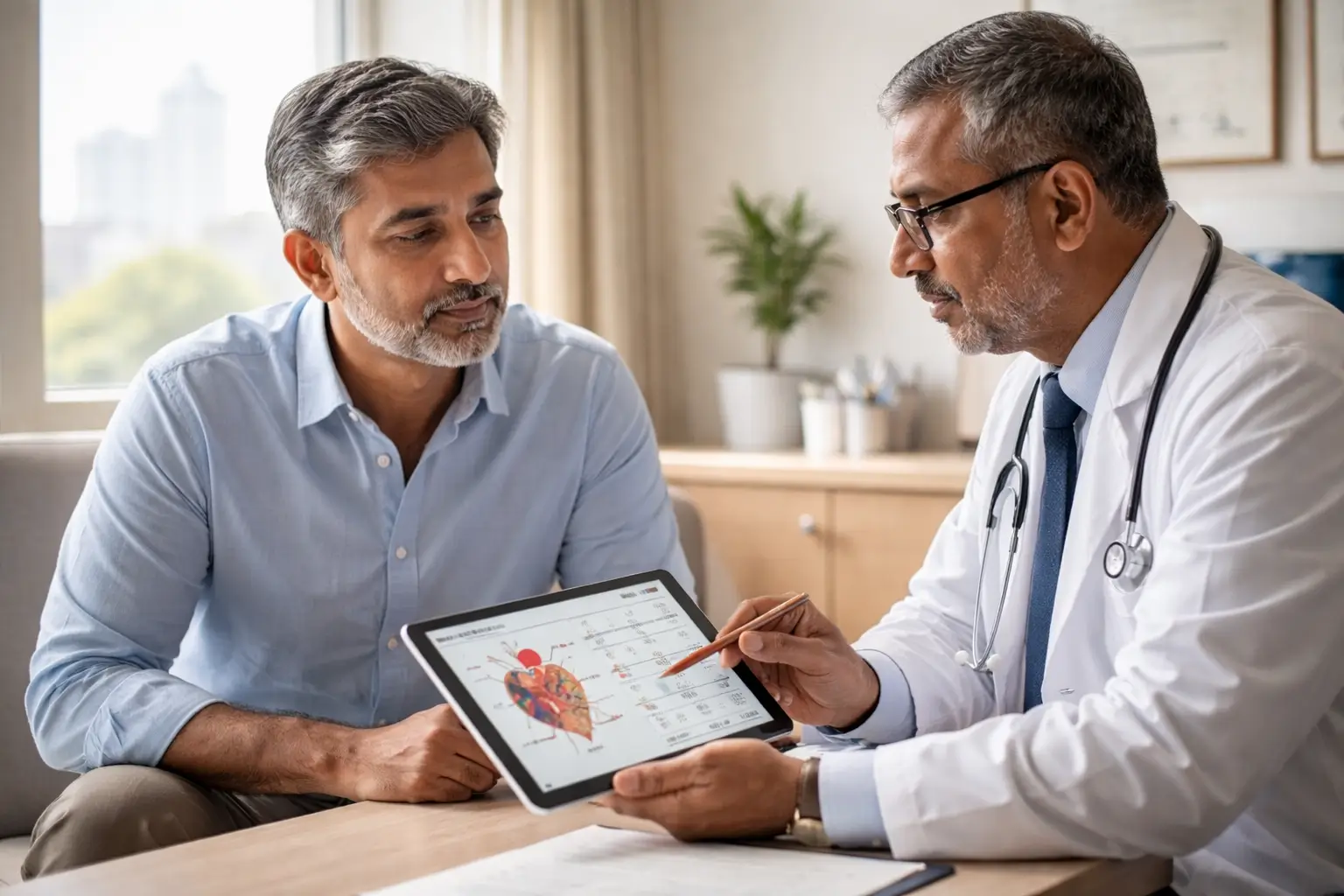
How doctors actually assess heart health
Understanding common tests reduces fear and confusion.
- Blood tests: cholesterol fractions, glucose, inflammatory markers
- Electrocardiogram (ECG): rhythm and electrical activity
- Echocardiogram: structure and pumping efficiency
- Stress testing: response to exertion
- Coronary calcium scoring (select cases): plaque burden
These tools are interpreted together—not in isolation—to guide decisions.
When prevention becomes treatment
Many people hesitate to start medication, fearing dependency. In reality, early treatment for blood pressure or cholesterol often prevents irreversible damage and may reduce medication needs later when combined with lifestyle changes.
Decisions should be individualized, considering:
- Absolute risk
- Age and comorbidities
- Response to non-pharmacological measures
Shared decision-making with a qualified clinician is central to truly knowing heart health.
Practical steps to know heart health better
Track key metrics annually—or more often if advised
Understand personal risk factors, not just population averages
Address sleep and stress as seriously as diet and exercise
Seek evaluation for persistent or unexplained symptoms
Avoid self-diagnosis or delayed care due to reassurance bias
The role of expert guidance
Guidelines from organizations such as World Health Organization and American Heart Association emphasize early risk identification, lifestyle modification, and evidence-based treatment. Their recommendations evolve with research—and responsible heart care evolves with them.
What knowing heart health really means
To know heart health is not to live in fear of disease. It is to recognize that prevention is quieter than crisis, and that informed attention today often prevents difficult decisions tomorrow. Ignoring signals rarely makes them disappear—but understanding them early often keeps them manageable.
Disclaimer
This article is for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding personal health concerns.